Among the most serious complications of laparoscopic and open cholecystectomy (gallbladder removal), is bile duct injury. According to healthcare experts, bile duct injury can greatly reduce the quality of life. The oft-used method for correction of this bile duct injury is the procedure called Roux-en-Y hepaticojejunostomy, which is in fact, the treatment of choice of a General Surgeon in Lahore. Read on to know more about this procedure:
What is hepaticojejunostomy?
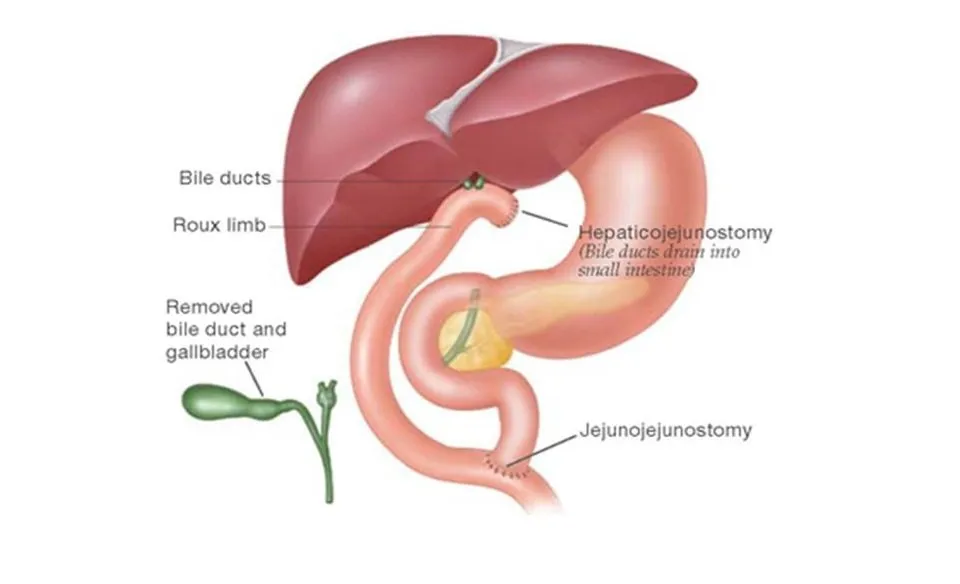
Hepaticojejunostomy is creation of a communication or anastomosis between the part of the small intestine called jejunum, and the hepatic duct—part of the bile flow tract. In normal circumstances, the bile flows from the hepatic duct in the liver, to the cystic duct (from the gall bladder) and together they form the common bile duct (CBD). This common bile duct then joins the duodenum (first part of the small intestine) and drains there.
If there is obstruction or injury to any part of the biliary system, the free flow of bile will be obstructed and in turn the liver will be affected, and digestion will be impaired. In such situations, hepaticojejunostomy is performed to ensure free flow of bile from the liver to the intestine.
Why is hepaticojejunostomy performed?
The major indications for hepaticojejunostomy are:
- Benign strictures in the biliary tract that may be congenital or due to stone, cysts or inflammation
- Stricture formation due to cholecystectomy
- Injury to the biliary tract during cholecystectomy (iatrogenic)
- Obstruction of the bile flow due to bile duct tumors
- Obstruction of the bile flow due to pancreatic tumors, especially head of pancreas
- Obstruction of bile flow due to gall bladder or liver tumors
- Trauma to the biliary tract
- Sclerosing cholangitis
- Choledochal cysts in the pediatric population
- Sometimes hepaticojejunostomy is performed for biliary tract reconstruction in liver transplant procedure
How is hepaticojejunostomy performed?
The procedure is performed under general anesthesia by a general surgeon. The surgery starts with incision to the abdomen, followed by cutting of the jejunum (second part of small intestine) about 30 cm away from end of duodenum or the first part of the small intestine. Thereafter, the lower part of the jejunum is taken close to the hepatic duct. The hepatic duct is cut just before it joins with the cystic duct to form the CBD. The jejunum is then joined with the hepatic duct with sutures. A drain is left in the place; the other end of the jejunum is connected with the more distal small intestine.
What are the risks of hepaticojejunostomy?
There are risks associated with all surgical procedures, as no procedure is fail-safe. The risks with hepaticojejunostomy are:
Risks associated with anesthesia
- Nausea
- Vomiting
- Confusion
- Headache
Risks associated with surgery
- Infection of the wound site
- Blood clots
- Hemorrhage—during or after the procedure
- Damage to nearby organs during the procedure
- Pneumonia in the post-surgery phase
Risks associated with the post-procedure stage
- Leakage of the anastomosis
- Formation of stricture
- Inflammation or infection of the peritoneum—peritonitis
- Abdominal abscess formation
- Collection of bile in the abdominal cavity—biloma
- Stone in the hepatic duct
- Inflammation of the hepatic duct
- Herniation through the incision
- Infection and sepsis
- Pancreatitis
What are the contraindications of hepaticojejunostomy?
Contraindications means the risk of procedure is quite high in such patients, and they need to be cleared in the preoperative physical examination to confirm their tolerance of the procedure. Contraindications for hepaticojejunostomy include:
- Severe cardiac dysfunction
- Severe pulmonary dysfunction
- History of systemic disorders
- Proximal obstruction to bile flow
What factors increase morbidity and mortality of hepaticojejunostomy?
According to the Best General Surgeon in islamabad, following factors increase the morbidity and mortality associated with this procedure:
- Male gender
- History of steroid use, as with autoimmune disorders
- History of uncontrolled diabetes
- Higher class in American Society of Anesthesiologists (ASA)
- Poor functional status according to pre-operative workup
- History of uncontrolled hypertension
- Also Read: Benefits of Mobile Apps for your Business.
Contents